Choice of the reconstruction material : Autogenous bone, Bone substitute, or Biomaterials?
Various materials can be used to rebuild the atrophied jaw :
- Autogenous bone : it is harvested from the patient’s own body on the day of jaw bone reconstruction.
- Allogenous bone : it comes from another human being’s body (Bank-bone)
- Xenogenous bone : it comes from other species (i.e animals, particularly bovine species)
- Bone substitute biomaterial of natural or synthetic origin.
The Choice of the grafting material depends on numerous factors :
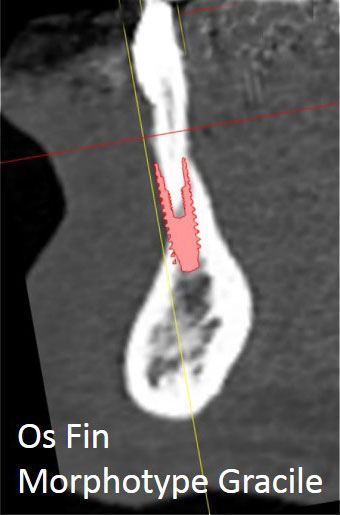
- The location, size and shape of the bone atrophy
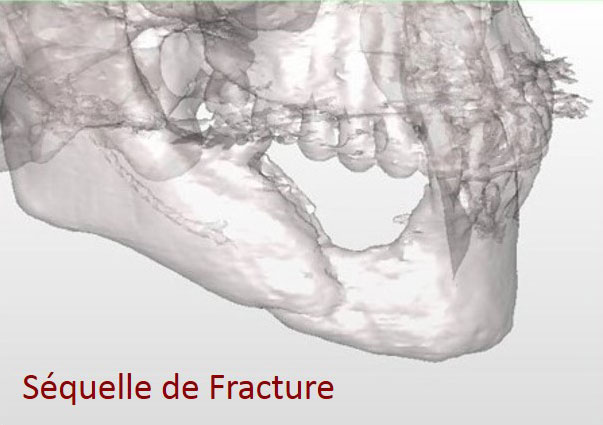
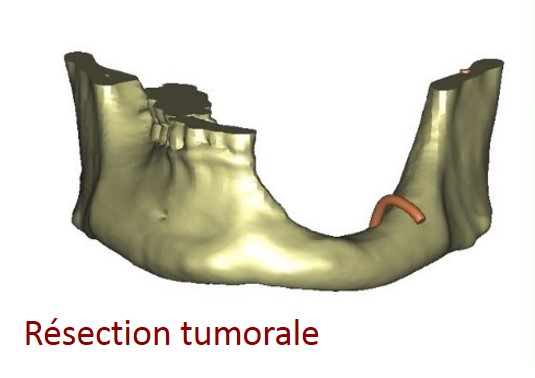
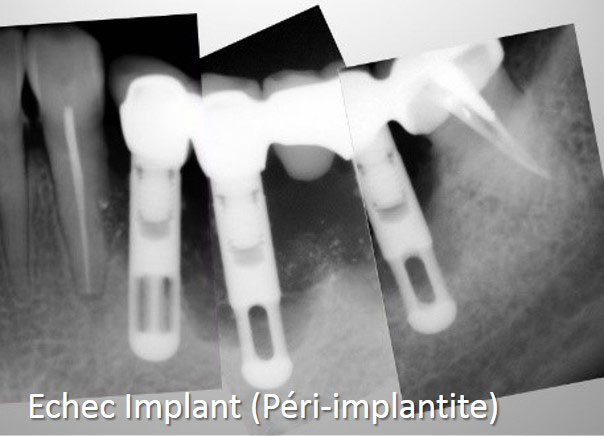
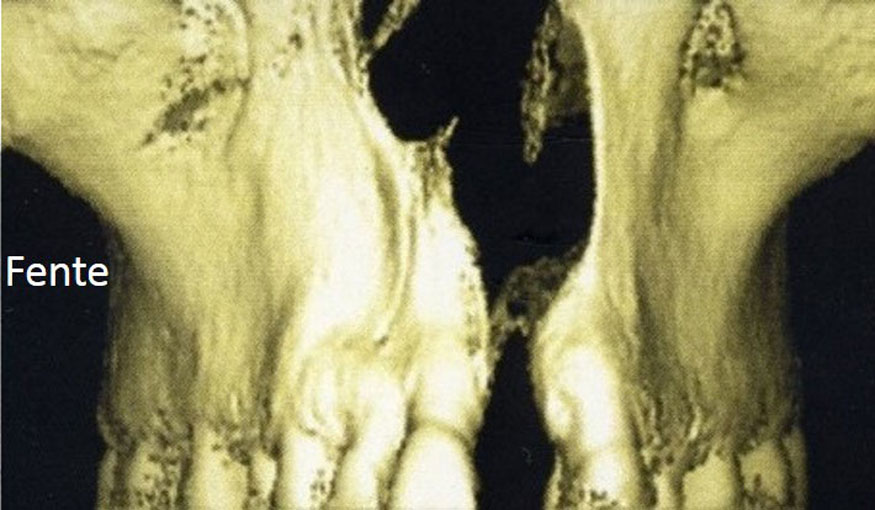
- The cause of the atrophy : ageing, periodontal disease, trauma, birth defect, tumor sequela….
- The quality of the gum tissue
- The patient’s medical profile (age, medical and surgical history…)
- The number and position planned for the implants.
Even though bone harvesting is required when performing autogenous bone grafting thus involving an extra surgical room, this procedure is still highly beneficial :
- The autogenous bone is harvested on the patient’s own body, therefore avoiding any infectious disease transmission (bacterial, virus, prion) and any immune mediated rejection.
- It is alive and already calcified during harvesting.
The autogenous bone is mostly used particularly in case of widespread atrophy.
There are numerous autogenous donor sites available. The reasons leading to the choice of a particular donor site or sites depend on the needs required for the reconstruction (quantity required, density, shape, etc.) and are explained thoroughly to the patient during the pre-operative consultations (informed consent).
Bone substitutes and biomaterials are beneficial as they avoid bone harvesting. They are most of the time used for small volume reconstructions or in addition to the autogenous bone in case of a large reconstruction. Bone substitutes authorized by the current French and European legislation show no risk of transmission of infectious disease (bacterial, virus, prion) or immune mediated rejection.
Whatever the reconstruction or material used, the patient will be explained thoroughly the criteria leading to the choice of procedure during the pre-operative consultation (informed consent)
Schedule. General treatment scheduling
Whatever the reconstruction procedure chosen, the steps in case of reconstruction are the following :
- Suppress any source of infection which may lead to reconstruction failure (removal of any remaining broken tooth or infected tooth, thorough dental scaling)
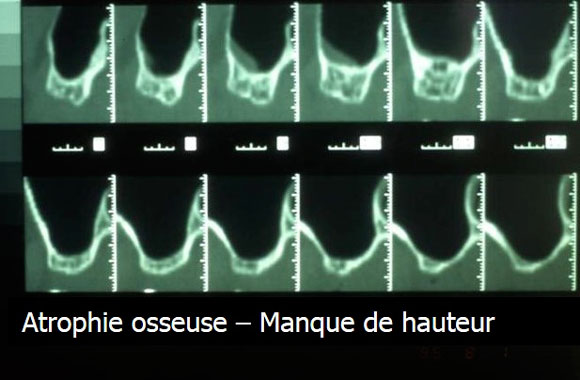
- Perform an X-ray in order to assess the bone loss and choose the most suitable type of reconstruction (height increase, thickness increase, mixed increase).
- Rebuild the bone volume
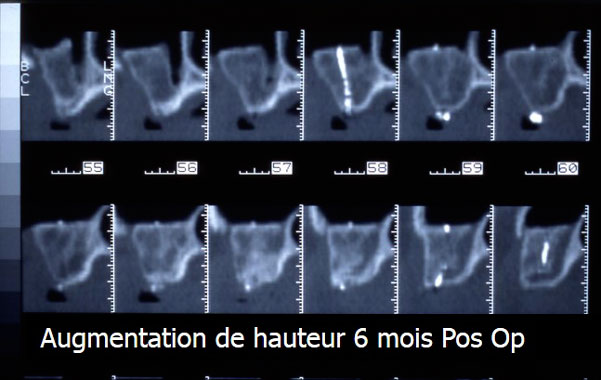
- Comply with a bone healing time of 5 to 6 months. During this step the patient may wear a removable denture provided it doesn’t compress the reconstructed area.
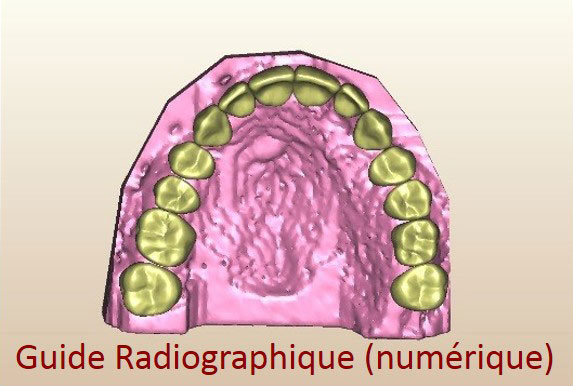
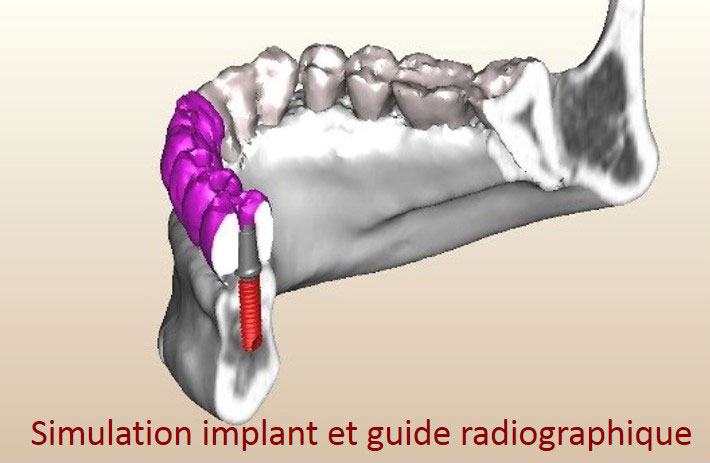
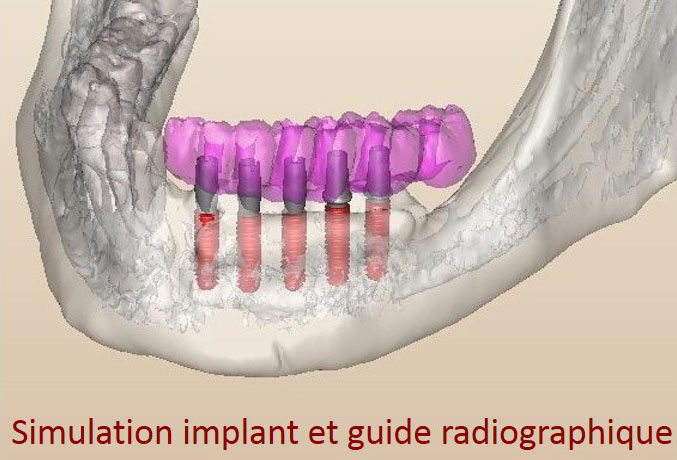
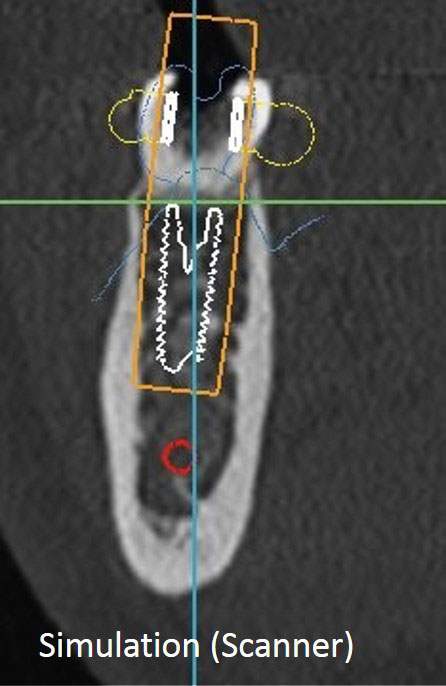
- Perform an Cone-Bean CT or CT Scan after the healing period to confirm the reconstruction in order to check the quality of the reconstruction and simulate the placement of the implants. The patient has a radiograph guide during the exam.
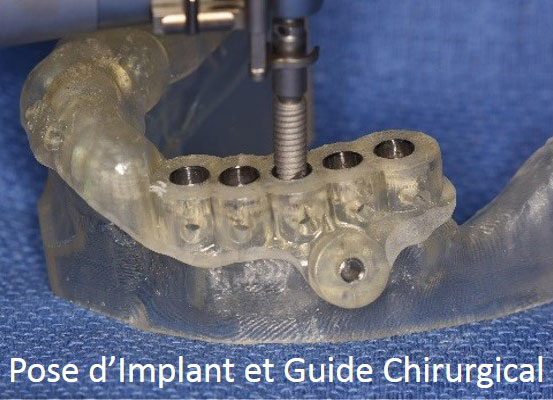
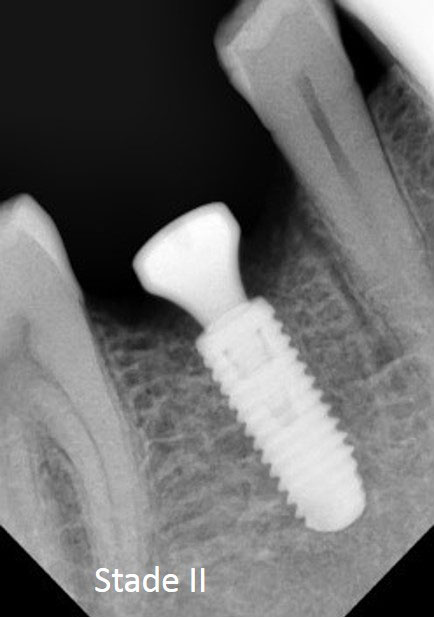
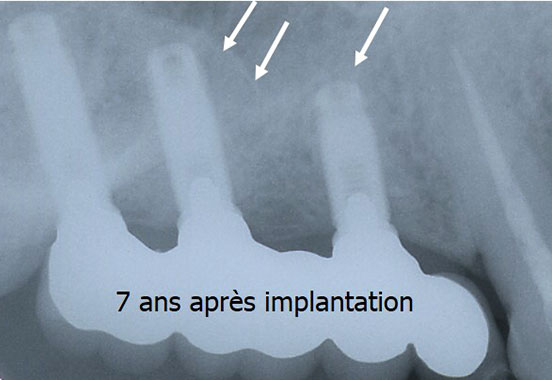
- Dental implant surgery
- Comply with an implant healing time of 2 to 6 months. During this step the patient may wear a removable denture provided it doesn’t compress the gengiva regarding the implants.
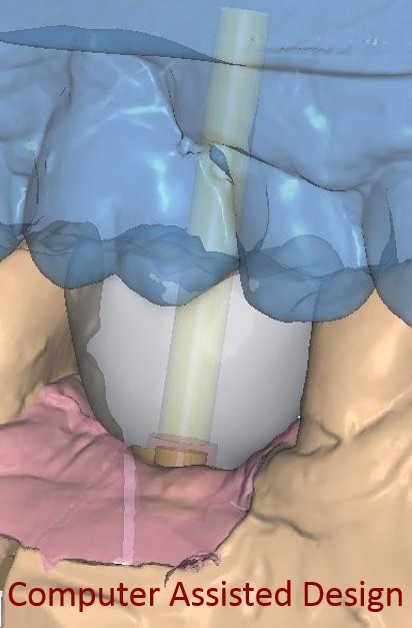
- Manufacture the dental prosthesis. Nowadays, to benefit from a greater accuracy to adapt dental prostheses to the underlying implants, the infrastructure of dental prostheses (crowns, bridges, etc.) is realized more and more thanks to computer softwares (CAD-CAM) (see videos).
Other Procedures and Associated Procedures
Osteotomies
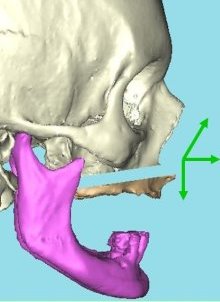
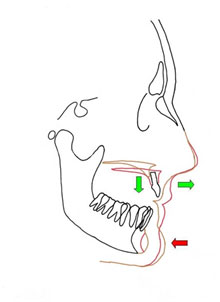
Osteotomies are designed to correct the abnormal distance between the two jaws. It is especially the case when edentulism is combined with alveolar bone loss. The space between the two jaws is too wide and prevents the production of a satisfactory implant prosthesis on a bio-mechanical level (the implants are too tilted or too short) or on a aesthetic level (a simulated gum tissue looks unsightly)
As in the jaw malformation surgery (see maxilla surgery or orthognathic surgery) osteotomies can deal with the whole skeleton of the jaw (complete osteotomies) or only one segment (segmental osteotomies).
The most frequent case is bone loss which is combined with complete edentulism of the upper maxilla. The resorbed toothless maxilla is located too far back compared to the mandible while the upper lip is set back as it is not supported. The distance between the upper maxilla and the lower maxilla is too wide. The surgical act consists of performing a Lefort 1 complete osteotomy moving the atrophied maxilla forward and downward while performing simultaneously a reconstruction of the bone structure using autogenous bones of iliac origin. This bone graft is placed in the intermediate space newly created by the forward and downward movement of the maxilla. Most of the time, onlay bone graft using autogenous bone of calvaria origin is performed jointly in order to thicken the maxillary crest which was too thin due to bone resorption phenomena.